You walk into a room, knowing you’re there for a reason, but within moments you’ve forgotten why you’re there. Some sufferers of HNPP claim to suffer from forgetfulness, memory blanks, and being in a haze. I write this completely woozy, the computer screen and mobile phone a complete blur, so it will be less detailed than usual.
“Brain fog” isn’t a medical condition in itself, rather a symptom of an underlying health issue or even a side effect from a medication. It can affect your ability to think and you may feel confused or disorganised or find it hard to focus or put your thoughts into words. It can be fleeting, but for others dealing with multiple chronic conditions, it tends to last longer.
While some individuals with HNPP may face this, it’s still questionable whether it is a direct symptom of this inherited disorder.
Watch HNPP sufferer Jessica Kellgren-Fozard speak about her experiences of brain fog:
Asked if memory problems such as forgetting words or conversations, as well as losing your train of thought are common occurrences with HNPP, Gareth Parry, M.D, appears to disagree.
According to HNPP.info, the Professor and Head, Department of Neurology, University of Minnesota, says: “I am not aware of forgetfulness being a problem with HNPP patients other than related to drugs. One of the commonest causes of forgetfulness in young people is distractibility. For example, when one is anxious about an exam or some such life crisis, one tends to forget the less pressing things associated with every day life.”
“It is a possibility, but I suppose there may also be some direct effect on the brain although the protein for which the gene encodes is not a CNS protein.”
– Gareth J. Parry, M.D
While he doesn’t completely discount it, he adds: “I frequently see patients with serious illnesses have major problems with memory. If HNPP is creating significant problems perhaps it is distracting the victim from their everyday activities. It is a possibility, but I suppose there may also be some direct effect on the brain although the protein for which the gene encodes is not a CNS [central nervous system] protein.”
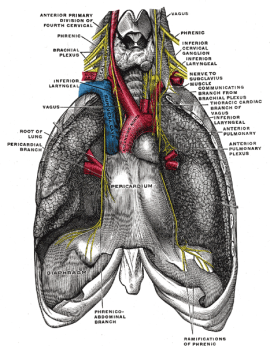
Cognitive fog may not be a direct symptom of HNPP, however, a 2013 study reports that some with either a duplication or deletion of the PMP22 gene, which is a fundamental tenet of the condition, had cognitive impairment.
Authors of the report Central Nervous System Abnormalities in Patients with PMP22 Gene Mutations said: “We found a decrease in the volume of WM [white matter] in 70% of patients, a reduced creatine level in WM in 28% and a cognitive impairment in 70%.”
White matter makes up half the human brain and has only recently been linked to cognition, the mental action or process of acquiring knowledge and understanding through thought, experience, and the senses. Research suggests that “white matter tracts mediate the essential connectivity by which human behaviour is organised, working in concert with grey matter to enable the extraordinary repertoire of human cognitive capacities.”
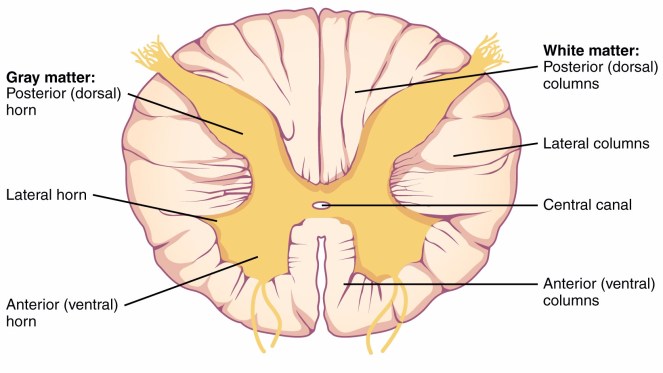
Writing in the Journal of Neurology, Neurosurgery, and Psychiatry, researchers of the above 2013 study say that the results showed that 47 per cent of the patients with HNPP and those with CMT1A had “abnormal” levels of white matter volume, creatine level in white matter as well as cognitive testing.
They conclude: “The study demonstrates that altered PMP22 gene expression induces significant CNS alterations in patients with HNPP and CMT1A, including cerebral WM abnormalities and cognitive impairment.”
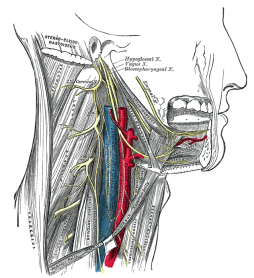
In the 2013 edition of Nervous System Diseases: New Insights for the Healthcare Professional, reporters from VerticalNews based in Strasbourg, France, reiterates the research, quoting the authors above: “Mutations of the peripheral myelin protein-22 (PMP22) gene are the most common cause of inherited diseases of the peripheral nervous system (PNS), with its deletion resulting in hereditary neuropathy with liability to pressure palsies (HNPP), and its duplication inducing Charcot Marie-Tooth 1A (CMT1A) diseases.
“Although mainly expressed in the PNS, PMP22 mRNA and protein are also present in the central nervous system (CNS).”
With only 30 participants tested in total, further research may be required for more definitive results.
What other causes could be a factor?
Medications
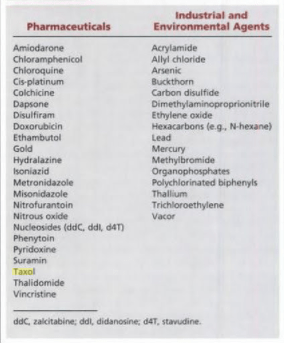
Some drugs – either prescribed or over the counter – can cause brain fog. If you take medicine and notice that your thinking isn’t as clear as it should be or you suddenly can’t remember things, it might be worth asking your medical practitioner if there is an alternative or if the side effects will pass.
Chronic Fatigue
An obvious part of feeling ‘foggy’ is dealing with chronic fatigue. With chronic fatigue, your body and mind are tired for a long time. You may feel confused, forgetful, and unable to focus.
Sleep
You need sleep to help your brain work the way it should, but too much can make you feel foggy, too. Aim for 7 to 9 hours.
Blogger Mark from Developing The Human Brain recommends allowing your body to wake up slowly and begin to move slowly. He adds: “Sit up in your bed for at least 12 sec after you wake up for stabilizing your blood flow.”
Dehydration
If you’re even the slightest bit dehydrated, it’s impossible to function at your full capacity. Every single cell in your body needs water, including those in your brain and your muscles. As the brain and heart is made up of 73 per cent water, it is the first organs to show signs of dehydration. Mild dehydration may affect your ability to take on mental tasks and cause you to feel foggy headed, according to a study from the British Journal of Nutrition.
Tips to reduce brain fog
- Sleep – get enough sleep at night and stick to a reasonable bedtime. Also, find ways to manage mental and emotional stressors, such as conscious breathing or purposeful exercise.
- Take note – either write down anything you need to do or create reminders and lists. Whether using post-it notes, a notebook, calendars or whatever works for you personally, all of these things help keep a record of what you need to remember.
- Ask for help – if you have people around you, ask them to remind you of anything important.
- Mobile apps – there are a whole host of mobile apps that can help you plan ahead including:
- Cozi – marketed as a “family app”, you can keep everyone’s activities and appointments; as well as create and share shopping lists, chores.
- MedCoach – medical app that helps you remember to take your medications and pills at the right time and day.
- Evernote – you can capture, organise, and share notes from anywhere including taking pictures, websites, and making voice notes. It can be synced as well.
- Todoist – like Evernote – automatically syncs wherever you log in, which is useful for those moments of clarity when you need to write something down quickly.
- Vitamin D – increased exposure to sunlight may help you to think more clearly. “The beauty of nature will give your prefrontal cortex – the area of your brain that helps you focus – an opportunity to recharge,” says neurologist Marie Palinski, at Massachusetts General Hospital.
- Flare-up tool kit – just like with chronic pain, you may need to put everything you need to help you make it through your flare in the same place/in a flare-up tool-kit box.
- Engage yourself – reading a book, seeing a play, or working a crossword puzzle or word game challenges your mind and stimulates your brain and your memory. Dr Palinski, also a faculty member at Harvard Medical School and author of Beautiful Brain, Beautiful You says, “When stuck in a rut, we’re constantly treading the same brain pathways. Engaging in a new activity literally wakes up our brains.” That’s because the brain has to lay new neural pathways to process new information. At the same time too much stimulation can be overwhelming.
- Postpone engagements – when you’re too tired and full of fog to think, put things off until the next day and get extra rest instead. Listen to the needs and signals your body gives. Use the presence of brain fog as a signal to slow down.
- Manage your environment – move to a quiet place to minimise distractions when you are trying to concentrate. Reducing clutter in your living space helps you to be more organised, and remember where things are. Create a daily routine for yourself. Sticking to a routine may help you remember what tasks you have to do each day, and in what order to do them.
- Relaxation techniques – relaxing activities such as yoga, tai chi and meditation can improve problems with sleep, fatigue, poor memory and anxiety – all of which are linked to brain fog, according to many studies.
While not everyone suffers from memory issues or general forgetfulness, it’s good to be prepared for any circumstance when you end up in a daze.